Antimicrobial resistance (AMR) has emerged as a formidable threat to public health, and the only way to effectively address it is through global collaboration. This issue demands the combined efforts of countries, international organizations, healthcare providers, and the research community.
Antimicrobial resistance occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve and become resistant to the drugs designed to kill them. This means that common infections that were once easily treatable with antibiotics or other antimicrobials can now become life-threatening. The overuse and misuse of antimicrobials in human medicine, veterinary medicine, and agriculture have contributed to the rapid spread of resistant strains. For example, in some parts of the world, antibiotics are prescribed unnecessarily for viral infections like the common cold, or used in large quantities in livestock farming to promote growth and prevent disease. As a result, resistant bacteria can spread from animals to humans through the food chain or direct contact.
The consequences of AMR are far-reaching. It leads to increased morbidity and mortality, longer hospital stays, and higher healthcare costs. Patients with resistant infections may require more expensive and toxic alternative treatments, and in some cases, there may be no effective treatment available. This not only affects individual patients but also strains healthcare systems. Moreover, AMR can have a significant impact on global health security, as it can lead to the emergence and spread of pandemics that are difficult to control.
No single country can solve the problem of AMR on its own. Global collaboration is essential for several reasons. First, it allows for the sharing of data and surveillance information. By pooling resources and knowledge, countries can better track the emergence and spread of resistant strains. Second, international cooperation is crucial in developing and implementing strategies to reduce the inappropriate use of antimicrobials. This could include setting global standards for antibiotic prescribing, promoting antibiotic stewardship programs, and regulating the use of antimicrobials in agriculture. Third, joint research efforts are needed to develop new antimicrobial agents and alternative treatment strategies. Scientists from different countries can collaborate to explore novel approaches such as phage therapy, immunotherapy, and the use of natural products with antimicrobial properties.
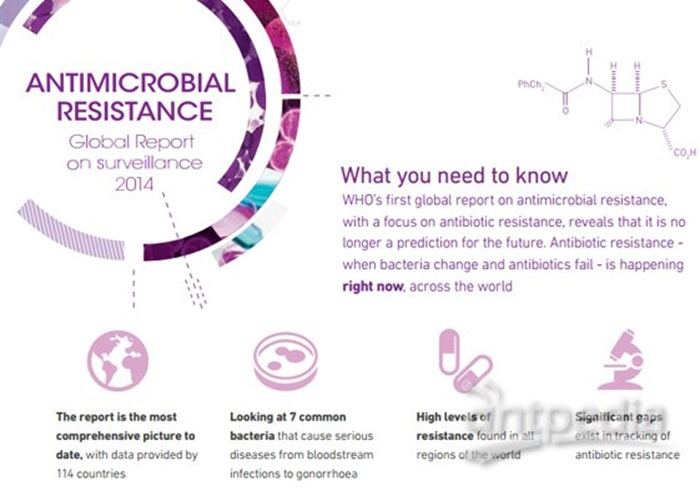
There are already some global initiatives in place to address AMR. The World Health Organization has launched a global action plan that includes measures such as improving surveillance, strengthening infection prevention and control, and promoting research and development. The G20 countries have also committed to taking action on AMR, including promoting the sustainable use of antimicrobials and enhancing international cooperation. However, more needs to be done. There is a need to increase funding for AMR research and to ensure that developing countries have the capacity to implement effective AMR strategies.
To effectively tackle AMR, all stakeholders must work together. Governments should enforce regulations on antimicrobial use and invest in public health infrastructure. Healthcare providers should adhere to evidence-based prescribing guidelines and educate patients about the proper use of antimicrobials. The public should also be aware of the risks of AMR and take steps to prevent the spread of infections, such as practicing good hygiene and getting vaccinated. Only through a coordinated global effort can we hope to slow down and reverse the trend of antimicrobial resistance and protect public health.
In conclusion, antimicrobial resistance is a global public health crisis that requires immediate and concerted global collaboration. By working together, we can safeguard the effectiveness of antimicrobials and ensure the health and well-being of future generations.
Read more
- Bacterial Vaginosis (BV): Causes and Treatment
- The Culprit: Understanding the Complex Causes of Sepsis
- The 5 Best Probiotic For Uti Female