Hormone replacement therapy (HRT) is a medical treatment that involves the use of hormones to supplement the body’s natural hormone levels. Urinary tract infections (UTIs), on the other hand, are common infections that affect the urinary system. The question of whether HRT can help with UTIs is an interesting one and requires a closer look at the relationship between hormones and the urinary tract.
Understanding UTIs
Causes and Symptoms
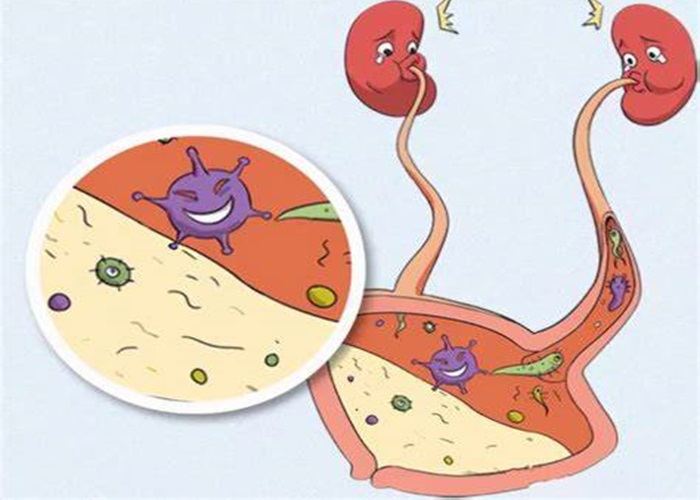
UTIs are typically caused by bacteria, most commonly Escherichia coli (E. coli), which enter the urinary tract through the urethra and multiply in the bladder. Women are more prone to UTIs than men due to their shorter urethra. Symptoms of a UTI can include a burning sensation during urination, frequent urination, an urgent need to urinate, and sometimes cloudy or bloody urine. In more severe cases, the infection can spread to the kidneys, leading to back pain, fever, and nausea.
The urinary tract has several defense mechanisms to prevent infections. These include the flow of urine, which helps to flush out bacteria, and the presence of certain substances in the urine that have antibacterial properties. However, factors such as poor hygiene, sexual activity, and certain medical conditions can disrupt these defenses and increase the risk of a UTI.
The Role of Hormones in the Urinary Tract
Estrogen and the Urogenital Tract
In women, estrogen plays a crucial role in maintaining the health of the urogenital tract. Estrogen helps to keep the lining of the bladder and urethra thick and healthy. It also promotes the production of substances like glycosaminoglycans, which form a protective layer on the bladder wall and prevent bacteria from adhering to it. As women age and enter menopause, estrogen levels decline, and this can lead to changes in the urogenital tissues.
The vaginal mucosa also becomes thinner and drier with decreased estrogen, which can increase the risk of UTIs. The proximity of the vagina to the urethra means that any changes in the vaginal environment can potentially affect the urethra and bladder. For example, a more alkaline vaginal pH due to reduced estrogen can encourage the growth of bacteria that are more likely to cause UTIs.
How HRT Might Impact UTIs
Estrogen – Based HRT
For post – menopausal women, estrogen – based HRT can potentially help reduce the risk of UTIs. By replenishing estrogen levels, HRT can improve the health of the bladder and urethral lining. This can lead to a thicker and more resilient mucosal layer, making it more difficult for bacteria to attach and cause an infection.
Some studies have shown that women on estrogen – based HRT have a lower incidence of recurrent UTIs. The form of HRT can also matter. Local estrogen therapy, such as vaginal estrogen creams or pessaries, can directly target the urogenital tissues. These forms of treatment can increase the local estrogen concentration in the vagina and urethra, providing a more immediate benefit in terms of reducing the risk of UTIs.
Hormonal Balance and Immune Function
HRT can also have an impact on the body’s overall hormonal balance, which in turn may affect the immune system. Estrogen has immunomodulatory effects and can enhance the body’s immune response to infections. By maintaining more stable hormone levels through HRT, the immune system may be better able to fight off bacteria that enter the urinary tract.
However, it’s important to note that HRT is not a one – size – fits – all solution and may have other potential risks and side – effects. For example, combined HRT (estrogen and progestogen) may have different effects compared to estrogen – only HRT. Progestogen can sometimes counteract the beneficial effects of estrogen on the urogenital tract and may even increase the risk of UTIs in some cases.
Considerations and Limitations
Risks Associated with HRT
While HRT may offer some benefits in terms of UTI prevention, it’s not without risks. Estrogen – based HRT has been associated with an increased risk of certain cancers, such as breast cancer and endometrial cancer (in women with a uterus). The decision to use HRT should always be carefully weighed against these potential risks, taking into account an individual’s medical history, family history of diseases, and other risk factors.
There can also be side – effects such as breast tenderness, bloating, and an increased risk of blood clots. These side – effects can vary depending on the type of HRT, the dosage, and the individual’s response to the treatment.
Alternative Approaches to UTI Prevention
Even if HRT shows some potential in helping with UTIs, it’s not the only option. Other preventive measures include maintaining good hygiene, drinking plenty of water to flush out bacteria, and urinating after sexual intercourse. Cranberry products have also been studied for their potential to prevent UTIs. Cranberries contain compounds that can prevent bacteria from adhering to the bladder wall.
For recurrent UTIs, antibiotics may be prescribed, but overuse of antibiotics can lead to antibiotic – resistant bacteria. Therefore, a combination of lifestyle changes and, in some cases, more targeted medical interventions may be a more appropriate approach than relying solely on HRT.
Conclusion
HRT, particularly estrogen – based HRT, may have a role in helping to prevent UTIs in post – menopausal women by improving the health of the urogenital tissues and potentially enhancing the immune response. However, the decision to use HRT for UTI prevention must be carefully considered in light of its potential risks and side – effects. Alternative strategies for UTI prevention should also be explored, and any treatment plan should be individualized based on a person’s specific health needs and circumstances.
Related topics:
Can You Get HRT Over The Counter(OTC)?
Why Taking Hrt Help With Weight Loss?
What Are The Alternatives To HRT?