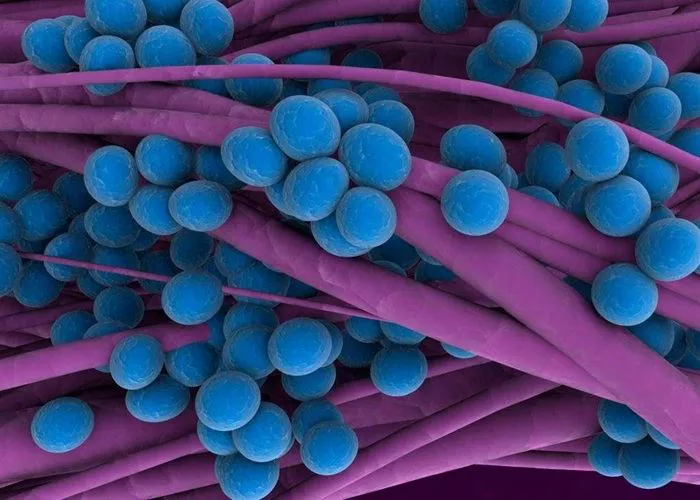
Staphylococcus aureus, commonly called staph, lives harmlessly on the skin of about one third of the population. This round-shaped bacterium only becomes dangerous when it enters the body through cuts or other openings. When this happens, it can cause infections ranging from minor skin problems to life-threatening conditions.
How Staph Infections Begin
The bacteria typically enter through broken skin. A small cut, surgical wound, or even a tiny crack from eczema provides enough opening. Once inside, the bacteria multiply rapidly. Your immune system may contain the infection or it may spread depending on the strain and your health status.
Staph produces various toxins and enzymes that damage tissue. Some strains release poisonous substances that cause food poisoning when contaminated food is eaten. Others generate toxins leading to toxic shock syndrome or scalded skin syndrome in severe cases.
These bacteria thrive in warm, moist environments. Gym equipment, towels, and razors can harbor staph and spread it between people. Hospitals pose particular risk because many patients have weakened immunity and surgical wounds that allow easy entry.
Common Types of Staph Infections
Skin infections represent the most frequent staph problems. Boils appear as red, swollen lumps filled with pus. They often develop in hair follicles or oil glands, becoming painful and warm to the touch. Impetigo causes crusty, honey-colored sores, mostly in children.
Cellitis makes skin red, swollen, and tender as infection spreads beneath the surface. Abscesses form pockets of pus that require drainage. These skin infections often start as small red bumps that quickly worsen without treatment.
Invasive staph infections occur when bacteria enter the bloodstream. Bacteremia leads to fever and low blood pressure as infection spreads throughout the body. Endocarditis damages heart valves, while osteomyelitis infects bones. Pneumonia fills lungs with fluid, making breathing difficult.
Recognizing Staph Infection Symptoms
Skin infections show obvious signs. The area becomes red, swollen, and painful. Pus-filled blisters may form and eventually burst. Warmth radiates from the infected spot as blood flow increases to fight the invaders.
Systemic infections cause fever and chills as your body tries to kill the bacteria. Fatigue sets in as your immune system works overtime. Muscle aches develop from inflammation throughout the body. Confusion may occur if infection reaches the brain.
Toxic shock syndrome brings sudden high fever, vomiting, and a sunburn-like rash. Blood pressure drops dangerously low as toxins overwhelm the system. This medical emergency requires immediate hospitalization and intensive care.
Who Gets Staph Infections
Anyone can develop staph infections, but some face higher risk. Hospital patients, especially those with open wounds or tubes entering their body, are particularly vulnerable. The bacteria spread easily in healthcare settings where many people have compromised immunity.
Athletes often contract staph through shared equipment and skin-to-skin contact. Sports involving cuts and abrasions like wrestling or football increase exposure. Gym users risk infection from improperly cleaned mats and weights.
People with chronic conditions like diabetes or vascular disease heal slower, giving staph more time to establish infection. Those with weakened immune systems from HIV, chemotherapy, or medications struggle to fight invading bacteria.
Children frequently get staph skin infections because their immune systems are still developing. Elderly individuals also face higher risk due to thinner skin and slower healing. Intravenous drug users introduce bacteria directly into their bloodstream through needles.
Diagnosing Staph Infections
Doctors often recognize staph skin infections by appearance alone. The characteristic redness, swelling, and pus point clearly to bacterial involvement. For deeper or systemic infections, testing becomes necessary.
Culture tests identify the specific bacteria causing infection. A swab of wound drainage or sample of blood, urine, or spinal fluid goes to the lab. Technicians grow the bacteria to determine the exact strain and which antibiotics will work best.
Blood tests reveal signs of infection throughout the body. Elevated white blood cell counts show your immune system is fighting invaders. Blood cultures detect bacteria circulating in your bloodstream.
Imaging locates hidden infections. X-rays find bone infections, while CT or MRI scans reveal abscesses in organs or deep tissues. Echocardiograms check heart valves for signs of endocarditis in serious cases.
Treating Staph Infections
Antibiotics remain the primary treatment for most staph infections. For minor skin infections, topical ointments like mupirocin often suffice. More serious cases require oral antibiotics such as cephalexin or clindamycin.
Severe or resistant infections may need intravenous antibiotics. Vancomycin has long been the go-to for serious staph, though newer options like linezolid and daptomycin now exist. Treatment duration ranges from days to weeks depending on infection severity.
Drainage proves crucial for abscesses and boils. Doctors make a small incision to let pus escape, then pack the cavity to keep it open as it heals. This relieves pressure and removes bacteria-laden fluid helping the infection spread.
Supportive care helps your body fight the infection. Rest allows energy to focus on healing. Hydration maintains blood pressure and flushes toxins. Pain relievers reduce discomfort while your immune system works.
The Challenge of MRSA
Methicillin-resistant Staphylococcus aureus resists many common antibiotics. This superbug emerged from overuse of antibiotics in medicine and agriculture. MRSA causes the same infections as regular staph but proves much harder to treat.
Hospital-acquired MRSA strains typically infect people with health problems. Community-associated MRSA spreads among healthy people outside healthcare settings. Both types require special antibiotics and sometimes lengthy hospital stays.
Preventing MRSA transmission requires strict hygiene. Healthcare workers must wash hands thoroughly between patients. Visitors should use alcohol-based sanitizers. Patients with MRSA may need isolation to protect others.
New antibiotics are being developed to combat resistant strains. Researchers are also exploring alternative treatments like bacteriophage therapy that uses viruses to kill bacteria. Vaccine development continues but has proven challenging so far.
Preventing Staph Infections
Good hygiene blocks most staph transmission. Wash hands frequently with soap and water, especially after touching potentially contaminated surfaces. Use alcohol-based sanitizers when washing isn’t possible.
Keep wounds clean and covered until fully healed. Change bandages regularly and dispose of used dressings properly. Avoid sharing personal items like towels, razors, or athletic equipment that may carry bacteria.
Shower after exercise or activities causing heavy sweating. Use clean towels to dry off completely, paying attention to skin folds where moisture lingers. Wear loose, breathable clothing to minimize skin irritation.
Disinfect surfaces regularly in homes and gyms. Pay special attention to high-touch areas like doorknobs and light switches. Follow manufacturer instructions for proper use of disinfectants to ensure they kill bacteria effectively.
When to Seek Medical Help
Minor skin infections may resolve with home care, but certain signs demand professional attention. Increasing pain, swelling, or redness indicates worsening infection. Red streaks extending from the wound suggest spreading infection through lymph vessels.
Fever accompanying skin changes signals systemic involvement. Chills, nausea, or confusion mean the infection may have entered your bloodstream. These symptoms require immediate evaluation to prevent life-threatening complications.
Recurrent infections suggest you may be a staph carrier. Your doctor can test for nasal colonization and prescribe special ointments to eliminate the bacteria from your body. Family members may need testing and treatment too.
Slow-healing wounds in diabetics or those with poor circulation often benefit from early antibiotic treatment. Waiting too long allows infection to become severe. Regular wound checks help catch problems before they escalate.
Living With Recurrent Staph Infections
Some people battle frequent staph infections despite precautions. Identifying and eliminating sources of reinfection becomes crucial. Pets can carry staph, so veterinary evaluation may be needed if infections persist.
Household cleaning must target staph reservoirs. Wash bedding and towels in hot water with bleach when possible. Disinfect surfaces regularly, especially in bathrooms and kitchens. Consider replacing old sponges and cleaning tools that harbor bacteria.
Diet may influence susceptibility. Some evidence suggests zinc and vitamin C support immune function against staph. Probiotics might help maintain healthy skin flora that outcompetes harmful bacteria. Discuss supplements with your doctor.
Stress management helps your immune system function optimally. Chronic stress weakens defenses against infection. Techniques like meditation, adequate sleep, and regular exercise may reduce recurrence frequency.
Complications of Staph Infections
Untreated staph infections can lead to serious problems. Sepsis occurs when infection overwhelms the bloodstream, causing organ failure. This medical emergency requires intensive care and powerful antibiotics.
Bone infections demand prolonged treatment. Osteomyelitis may need weeks of IV antibiotics followed by oral medications. Severe cases require surgery to remove infected bone tissue. Joint replacements can become infected years after implantation.
Heart valve damage from endocarditis sometimes requires surgical repair. The infection scars valves, preventing proper blood flow. Artificial valves may be needed to restore normal heart function after clearing the infection.
Toxic shock syndrome causes multi-organ damage even after the infection clears. Kidneys, liver, and heart may need time to recover function. Some patients experience long-term effects like muscle weakness or memory problems.
Special Considerations for Children
Children’s developing immune systems handle staph differently. Scalded skin syndrome primarily affects infants and young children. The bacteria release toxins causing widespread skin peeling that resembles burns.
School outbreaks sometimes occur with MRSA. Shared toys, sports equipment, and close contact facilitate spread. Schools should implement cleaning protocols and educate students about proper hygiene.
Parents should monitor minor scrapes and cuts closely. Children may not report early symptoms. Look for increasing redness, swelling, or pain at injury sites. Fever or behavior changes may indicate spreading infection.
Pediatric treatment often involves liquid antibiotics. Dosage is carefully calculated by weight. Completing the full course is essential even if symptoms improve quickly to prevent recurrence and resistance.
Conclusion
Researchers are developing new approaches to combat staph. Vaccine trials continue, though creating an effective vaccine has proven difficult due to the bacteria’s complexity and multiple strains.
Alternative therapies show promise. Manuka honey has natural antibacterial properties useful for wound care. Essential oils like tea tree oil are being studied for topical use against antibiotic-resistant strains.
Phage therapy uses viruses that specifically target bacteria. These bacteriophages evolve alongside bacteria, potentially overcoming resistance. Clinical trials are exploring this century-old concept with modern technology.
Improved diagnostics aim to identify infections faster. Rapid tests could detect staph and its antibiotic resistance within hours rather than days. This would allow targeted treatment sooner, improving outcomes.
Related topics:
How To Get Rid Of Bacterial Infection In Nose?
Bacterial Infections on the Lips: Causes, Symptoms & Treatment