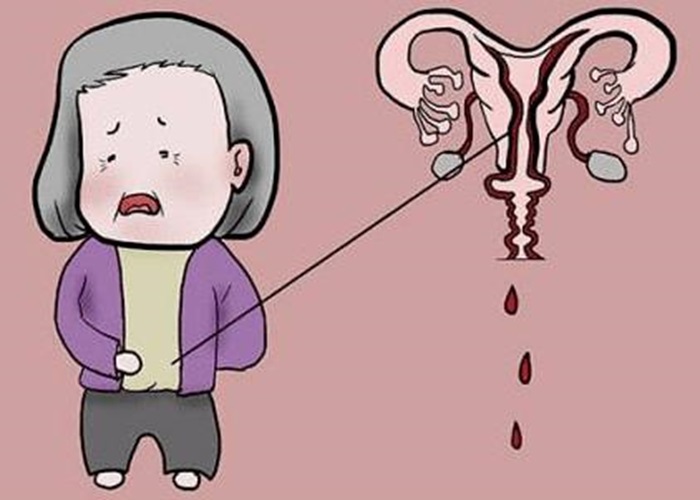
Menopause is a natural process that marks the end of a woman’s reproductive years. It is defined as the absence of menstrual periods for 12 consecutive months. While menopause is a normal part of aging, it can also be accompanied by a variety of symptoms, including hot flashes, mood changes, and vaginal dryness. One symptom that can be concerning for women after menopause is spotting or bleeding.
Symptoms of Spotting After Menopause
Spotting after menopause is defined as any vaginal bleeding that occurs after a woman has gone 12 consecutive months without a menstrual period. The bleeding may be light or heavy, and may be accompanied by other symptoms, such as:
Pain or discomfort: Some women may experience pain or discomfort during or after spotting.
Vaginal discharge: Some women may experience vaginal discharge, which may be bloody or brown in color.
Cramping: Some women may experience cramping or abdominal pain during or after spotting.
Fatigue: Some women may feel tired or fatigued after spotting.
The symptoms of spotting after menopause can vary depending on the underlying cause. In some cases, women may experience only light spotting or bleeding. In other cases, the bleeding may be heavy and prolonged. Other symptoms may include:
- Pain or discomfort during sexual intercourse
- Vaginal dryness or itching
- Abdominal pain or cramping
- Fatigue or weakness
- Loss of appetite or weight loss
Understanding Post-Menopausal Spotting
Post-menopausal spotting refers to any vaginal bleeding that occurs after a woman has gone through menopause. It is not uncommon for women to experience some light spotting or bleeding during the first year after menopause. However, if the spotting continues or becomes heavier, it may be a sign of a more serious condition.
Causes of Spotting After Menopause
There are several possible causes of spotting after menopause. These include:
Vaginal atrophy: Vaginal atrophy is a condition that occurs when the walls of the vagina become thin, dry, and less elastic. This is due to a decrease in estrogen levels, which occurs naturally during menopause. The lack of estrogen causes the vaginal tissues to become less hydrated, leading to dryness and thinning of the vaginal walls. This can cause vaginal bleeding or spotting, especially after sexual intercourse.
Hormone therapy: Hormone therapy is a treatment that involves taking estrogen and/or progesterone to relieve menopausal symptoms. However, it can sometimes cause vaginal bleeding or spotting.
Endometrial cancer: This is a type of cancer that affects the lining of the uterus. It can cause abnormal vaginal bleeding, including spotting after menopause.
Polyps: Polyps are growths that can develop in the uterus or cervix. They can cause vaginal bleeding or spotting, especially after sexual intercourse.
Infections: Certain infections, such as bacterial vaginosis or yeast infections, can cause vaginal bleeding or spotting.
When to See a Doctor
If you experience spotting or bleeding after menopause, it is important to see a doctor. Your doctor will perform a physical exam and may recommend additional tests, such as a pelvic ultrasound or biopsy, to determine the cause of the spotting. If the cause is vaginal atrophy, your doctor may recommend using a vaginal moisturizer or lubricant to relieve dryness and reduce the risk of bleeding. Hormone therapy may also be recommended to increase estrogen levels and improve vaginal health. If the cause is more serious, such as endometrial cancer, your doctor may recommend surgery, radiation therapy, or chemotherapy.
Prevention of Spotting After Menopause
While some causes of spotting after menopause cannot be prevented, there are steps that women can take to reduce their risk. These include:
- Maintaining a healthy weight
- Exercising regularly
- Eating a healthy diet
- Quitting smoking
- Limiting alcohol consumption
- Practicing safe sex
- Seeing a doctor regularly for check-ups and screenings
In conclusion, spotting after menopause can be a cause for concern, as it may indicate an underlying medical condition. While vaginal atrophy is the most common cause, there are other potential causes that should be considered. If you experience spotting or bleeding after menopause, it is important to see a doctor to determine the cause and receive appropriate treatment. Women can also take steps to reduce their risk of spotting after menopause by maintaining a healthy lifestyle and seeing a doctor regularly for check-ups and screenings.
Treatment Options for Spotting After Menopause
The treatment for spotting after menopause depends on the underlying cause. If the cause is hormonal changes or vaginal atrophy, treatment may include:
Vaginal estrogen: Vaginal estrogen can help to thicken and lubricate the vaginal tissues, which can reduce the risk of spotting.
Lubricants: Lubricants can help to reduce vaginal dryness and discomfort during intercourse.
Lifestyle changes: Certain lifestyle changes, such as quitting smoking and maintaining a healthy weight, can also help to reduce the risk of spotting after menopause.
If the cause of spotting after menopause is polyps or endometrial cancer, treatment may include:
Surgery: Surgery may be necessary to remove polyps or cancerous tissue.
Radiation therapy: Radiation therapy may be used to treat endometrial cancer.
Chemotherapy: Chemotherapy may be used to treat endometrial cancer that has spread to other parts of the body.
If the cause of spotting after menopause is medication, a healthcare provider may recommend adjusting the dosage or switching to a different medication.
Conclusion
Spotting after menopause can be a concerning symptom for women. While there are several possible causes of spotting after menopause, the most common cause is hormonal changes and vaginal atrophy. Other causes include polyps, endometrial cancer, and certain medications. Treatment options for spotting after menopause depend on the underlying cause and may include vaginal estrogen, lubricants, surgery, radiation therapy, chemotherapy, or medication adjustments. It is important for women who experience spotting after menopause to discuss their symptoms with a healthcare provider to determine the best course of treatment. With proper treatment, women can manage their symptoms and improve their overall well-being.
Related topics: