Attention-deficit/hyperactivity disorder (ADHD) is commonly misunderstood, often being confused with mood disorders or personality disorders. It’s crucial to understand ADHD for what it truly is and how it affects those who live with it. In this article, we will explore whether ADHD is classified as a mood disorder or a personality disorder, clarify common misconceptions, and offer insights on managing and treating this condition.
Understanding ADHD: What Is It?
ADHD is a neurodevelopmental disorder that affects both children and adults, characterized by symptoms like inattention, hyperactivity, and impulsivity. It is not a mood disorder, which primarily affects a person’s emotional state (e.g., depression or bipolar disorder), nor is it a personality disorder, which involves enduring patterns of thought and behavior that deviate significantly from societal expectations (e.g., borderline personality disorder).
Common Symptoms of ADHD:
Inattention: Difficulty staying focused, forgetfulness, and distractibility.
Hyperactivity: Excessive fidgeting, restlessness, or difficulty staying seated.
Impulsivity: Acting without thinking, interrupting conversations, or making hasty decisions.
While these symptoms can overlap with other conditions, ADHD is distinct and has its own diagnostic criteria.
ADHD and Mood Disorders: Are They Linked?
Mood disorders, such as depression or bipolar disorder, primarily involve emotional regulation problems. A person with a mood disorder might experience extreme sadness, irritability, or even periods of mania. ADHD, however, is not directly related to these mood fluctuations but can co-occur with mood disorders.
Why ADHD and Mood Disorders Are Often Confused:
Emotional Dysregulation: Many people with ADHD experience challenges with emotional control, such as frustration, irritability, and impulsiveness. These behaviors can look similar to symptoms of mood disorders.
Co-occurrence: Research shows that people with ADHD are at higher risk of developing mood disorders, particularly depression or anxiety, due to the challenges of managing ADHD symptoms in everyday life.
Even though both conditions involve challenges with emotional regulation, ADHD itself is not classified as a mood disorder.
ADHD vs. Personality Disorders: What’s the Difference?
Personality disorders are mental health conditions where individuals exhibit deeply ingrained patterns of behavior that diverge from the norm. These behaviors often lead to distress or dysfunction. Common personality disorders include borderline personality disorder, narcissistic personality disorder, and antisocial personality disorder.
ADHD is different from personality disorders in several important ways:
Duration of Symptoms: Personality disorders typically emerge during adolescence or early adulthood and are chronic. ADHD symptoms usually present in childhood and may persist into adulthood, but they are not as enduring or pervasive in nature as personality disorders.
Pattern of Behavior: People with personality disorders may have consistent and long-standing patterns of dysfunctional behavior that affect relationships and work. ADHD, however, primarily impacts concentration, attention, and impulse control, which can vary depending on the situation.
It’s important to note that someone with ADHD may develop characteristics similar to those seen in a personality disorder, but this does not mean they have one. For example, impulsivity in ADHD can lead to poor decisions, but this is different from the pervasive instability seen in borderline personality disorder.
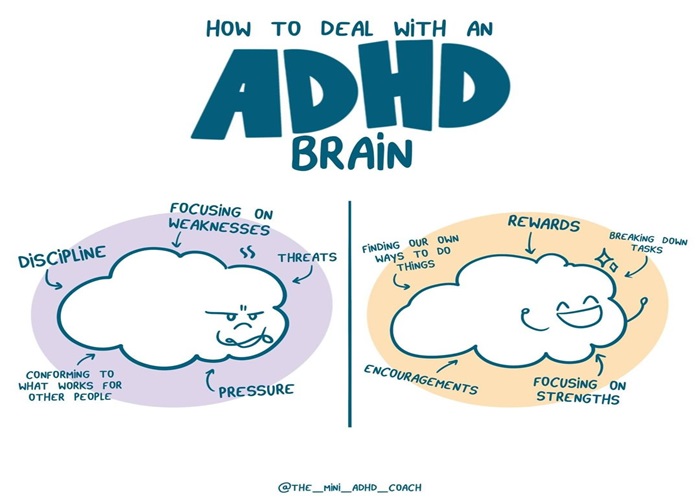
How to Manage ADHD and Co-occurring Conditions?
Managing ADHD requires a comprehensive approach that may involve behavioral therapy, medication, and lifestyle adjustments. For individuals who have both ADHD and a mood disorder or personality disorder, treatment should address both conditions simultaneously to improve overall well-being.
Key Strategies for Managing ADHD:
Medication: Stimulant medications like Adderall or Ritalin are commonly prescribed for ADHD and can help regulate attention and impulse control. Non-stimulant medications may be used in certain cases.
Behavioral Therapy: Cognitive-behavioral therapy (CBT) can help people with ADHD improve their organization skills, time management, and emotional regulation.
Lifestyle Changes: Regular exercise, a structured routine, and mindfulness practices can support emotional balance and improve focus.
For individuals with co-occurring mood or personality disorders, a tailored treatment plan that includes therapy and medication can help manage both ADHD and the other condition effectively.
FAQs
1. Can ADHD be mistaken for a mood disorder?
Yes, ADHD can sometimes be mistaken for a mood disorder because of symptoms like irritability, emotional instability, and impulsivity. However, ADHD is primarily a neurodevelopmental disorder and not a mood disorder.
2. How can ADHD affect daily life?
ADHD can impact various aspects of life, including work, relationships, and self-esteem. Individuals may struggle with maintaining attention at work, completing tasks on time, and regulating their emotions in social situations.
3. Is there a cure for ADHD?
There is currently no cure for ADHD, but the symptoms can be managed with a combination of medication, therapy, and lifestyle changes. Early intervention and treatment can significantly improve outcomes for individuals with ADHD.
Conclusion
ADHD is neither a mood disorder nor a personality disorder; it is a neurodevelopmental condition that impacts attention, impulse control, and hyperactivity. While it can co-occur with mood disorders and personality disorders, it is a distinct diagnosis that requires specific treatment approaches. If you or someone you know is struggling with ADHD, seeking professional guidance from a healthcare provider can help improve focus, emotional regulation, and overall quality of life.
Related articles:
- Is ADHD Genetic Or Environmental?
- Is ADHD A Intellectual Disability?
- Is Autism Related To ADHD: All You Need To Know