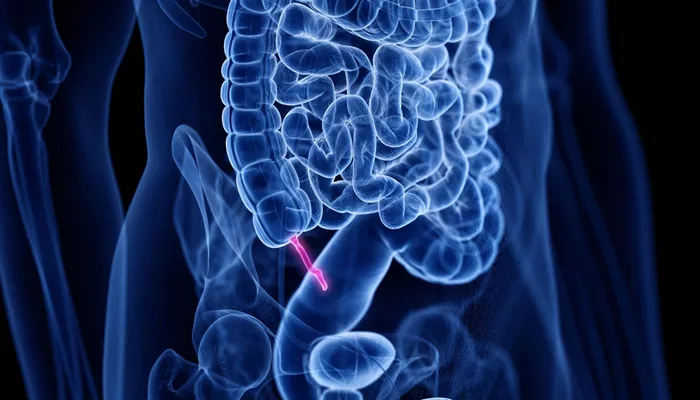
An appendix on the verge of bursting creates a medical emergency requiring immediate attention. The small pouch extending from the large intestine can become dangerously inflamed, leading to a condition called appendicitis that may progress to rupture. Recognizing the warning signs of impending rupture helps prevent life-threatening complications.
Understanding Appendix Rupture Risk
The appendix can burst when inflammation blocks its opening, trapping bacteria inside. As pressure builds from multiplying bacteria and swelling tissues, the wall weakens until it tears. This typically happens 48-72 hours after symptoms first appear, though timing varies by individual.
Rupture spreads infection throughout the abdomen in a condition called peritonitis. The risk increases when appendicitis goes untreated, making early recognition crucial. Certain symptoms suggest the appendix is nearing this dangerous point of no return.
Escalating Pain Patterns
Appendix pain changes character as rupture approaches. What begins as vague discomfort near the belly button intensifies and shifts to the lower right abdomen. The pain typically becomes constant and sharper as inflammation worsens.
A temporary pain decrease sometimes occurs right before rupture as pressure releases from the dying appendix wall. This false improvement quickly gives way to much worse pain as infection spreads. Any such fluctuation in pain severity warrants emergency evaluation.
Fever Spikes and Chills
While appendicitis often causes mild fever initially, a sudden temperature rise above 102°F (39°C) suggests possible rupture. The body mounts a stronger immune response as bacteria escape into the abdominal cavity. Chills and shaking may accompany this fever as the infection spreads.
Fever that develops after several hours of abdominal pain is particularly concerning. The combination of worsening pain with rising fever creates a red flag scenario needing urgent medical intervention.
Changes in Abdominal Firmness
The abdomen often becomes rigid and extremely tender as rupture nears. Light touch may cause intense pain as the protective membrane lining the abdomen becomes inflamed. The stomach muscles may involuntarily contract to guard the area, creating a board-like stiffness.
Pressing on the left lower abdomen sometimes causes right-sided pain (Rovsing’s sign), indicating advanced inflammation. Coughing or sudden movements typically intensify the discomfort at this stage. These physical changes reflect spreading irritation within the abdominal cavity.
Digestive System Shutdown
Nausea and vomiting often worsen as rupture becomes imminent. The digestive system essentially stops working, leading to inability to keep down even small sips of water. Bowel movements may cease completely as intestinal paralysis sets in.
Loss of appetite becomes absolute – the thought of food may trigger disgust. These gastrointestinal symptoms reflect the body’s emergency response to severe infection and impending abdominal catastrophe.
Mental Status Changes
As toxins spread from a rupturing appendix, mental function often deteriorates. Confusion, disorientation, or extreme lethargy may develop. Some patients become unusually agitated or combative as sepsis begins affecting brain function.
These neurological symptoms indicate systemic infection requiring intensive medical care. They often develop alongside other signs of rupture like rapid heartbeat and shallow breathing. Mental changes should never be ignored in someone with abdominal pain.
Rapid Heartbeat and Breathing
The heart rate accelerates as the body tries to circulate more blood to fight spreading infection. Pulse may exceed 100 beats per minute even at rest. Breathing becomes faster and shallower as the diaphragm reacts to abdominal inflammation.
These vital sign changes reflect the body’s escalating stress response. They often precede full septic shock, making their recognition potentially life-saving. Any such developments in someone with appendicitis symptoms demand emergency care.
When Minutes Matter
Appendix rupture creates a true medical emergency where delays can prove fatal. The infection spreads rapidly once the wall tears, causing blood pressure drops and organ failure. Survival rates decrease significantly after rupture occurs.
Emergency surgery becomes necessary to remove the burst appendix and clean the abdominal cavity. Powerful intravenous antibiotics are required to control widespread infection. These interventions work best when started before complete rupture happens.
Diagnostic Confirmation Methods
Doctors use several tools to assess rupture risk. Blood tests show elevated white blood cells and inflammatory markers. CT scans provide detailed images of appendix wall integrity. Ultrasound can detect abscess formation near the appendix.
Physical exam findings like rebound tenderness (pain upon releasing abdominal pressure) suggest advanced inflammation. These diagnostic tools help surgeons determine whether rupture has occurred or is imminent, guiding treatment decisions.
High-Risk Patient Groups
Some people face greater rupture risks. Young children often rupture faster due to narrower appendix openings. Elderly patients may delay seeking care, allowing more time for rupture. Those with compromised immune systems progress quicker to severe infection.
Individuals who ignore early symptoms or mistake appendicitis for stomach flu risk delayed diagnosis. People with atypical appendix positions may experience unusual symptoms that get overlooked initially. These groups require extra vigilance.
What Not to Do
Certain actions can accelerate rupture or mask symptoms. Never apply heat to the painful area as this increases blood flow and swelling. Avoid pain medications that might disguise symptom progression. Don’t eat or drink in case emergency surgery is needed.
Laxatives or enemas increase pressure in the digestive tract dangerously. Home remedies cannot stop the inflammatory process once it reaches critical stages. These interventions risk worsening the situation rather than helping.
Prevention Through Early Action
The only reliable way to prevent appendix rupture is seeking medical care at the first signs of appendicitis. Early surgical removal of the inflamed appendix is routine and safe. Laparoscopic techniques allow faster recovery with minimal scarring.
Antibiotics sometimes treat very early, mild cases without surgery. However, once moderate symptoms develop, surgery remains the gold standard. Prompt action prevents the much more serious consequences of rupture and peritonitis.
Final Thoughts
Recognizing the signs of impending appendix rupture can mean the difference between routine treatment and life-threatening complications. The progression from early appendicitis to rupture follows a predictable pattern that observant patients can detect.
When symptoms suggest rupture may be near, emergency medical attention becomes imperative. Modern medicine handles appendicitis effectively when caught early, making awareness of these warning signs potentially life-saving knowledge for everyone.
Related topics:
- How Do They Check Your Appendix?
- What Are Signs Of A Bad Appendix?
- How Long After Appendix Surgery Can You Have Intercourse?