Many people over 60 have small pouches in their colon walls and don’t even know it. This common condition called diverticulosis affects about half of adults by age 60 and nearly everyone by 80. While it sounds concerning, most people with these pouches experience no symptoms at all. Understanding what diverticulosis really means can help you manage your digestive health without unnecessary worry.
The Anatomy of Diverticulosis
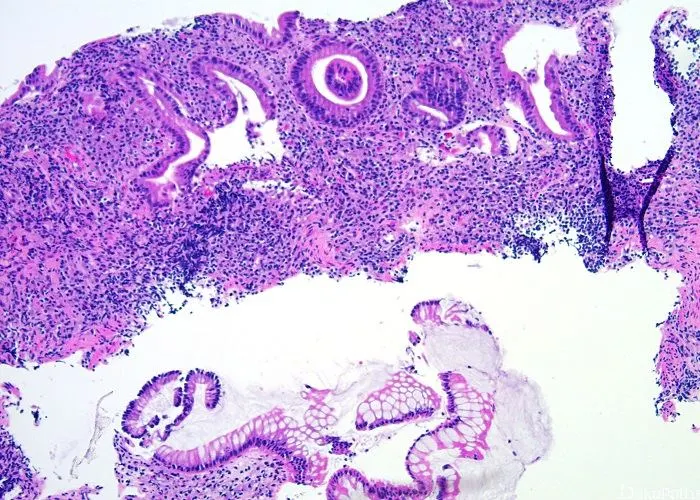
Diverticulosis occurs when small, bulging pouches develop in the digestive tract, most commonly in the lower part of the large intestine. These pouches, called diverticula, form when weak spots in the colon wall give way under pressure. Imagine a bicycle tire with thin spots that bulge outward when inflated – that’s similar to how diverticula form in the intestinal wall.
Each pouch typically measures between 5-10 millimeters in diameter, about the size of a pea. They rarely cause problems unless they become inflamed or infected, which is a different condition called diverticulitis. The presence of these pouches alone without symptoms is what doctors refer to as diverticulosis.
Why These Pouches Develop
The exact cause remains unclear, but doctors believe multiple factors contribute. A low-fiber diet appears to play a major role. Without enough fiber, stools become hard and difficult to pass. This increases pressure inside the colon as muscles work harder to move waste along. Over years, this constant pressure may push the inner lining through weak spots in the colon wall.
Aging also contributes naturally as colon walls weaken over time. Some people may inherit a tendency to develop diverticula. Obesity, lack of exercise, smoking, and certain medications like steroids and opioids may increase risk. Interestingly, diverticulosis is rare in countries where people eat high-fiber diets, supporting the dietary connection.
How Doctors Discover Diverticulosis
Most people discover they have diverticulosis incidentally during tests for other issues. Since it rarely causes symptoms, the condition often goes undetected for years. A colonoscopy frequently reveals these pouches as small dimples in the colon wall. CT scans and barium enema X-rays can also show diverticula.
Doctors don’t typically screen specifically for diverticulosis because finding it without symptoms doesn’t change medical care. If you experience persistent digestive symptoms, your doctor may order these tests to check for diverticulosis along with other possible conditions.
Common Misconceptions About the Condition
Many people confuse diverticulosis with its more serious cousin diverticulitis. Having diverticulosis doesn’t mean you’ll automatically develop diverticulitis – only about 5% of people with diverticulosis ever experience complications. Another myth suggests avoiding nuts, seeds, and popcorn, but research shows these foods don’t increase risk as previously believed.
Some patients worry the pouches might turn cancerous, but diverticulosis doesn’t increase colon cancer risk. The pouches themselves are harmless unless they become infected or rupture. Understanding these facts can prevent unnecessary dietary restrictions or anxiety about the condition.
Potential Symptoms When They Occur
While most people notice nothing, some with diverticulosis experience mild symptoms. These may include occasional bloating, abdominal discomfort (especially in the lower left side), or changes in bowel habits like constipation. The discomfort often eases after passing gas or having a bowel movement.
These vague symptoms overlap with many other digestive conditions like irritable bowel syndrome. If symptoms persist or worsen, they might signal developing complications rather than simple diverticulosis. Severe pain, fever, or rectal bleeding always warrant immediate medical attention.
Possible Complications to Watch For
Though uncommon, complications can arise. Diverticulitis occurs when pouches become inflamed or infected, causing significant pain, fever, and digestive upset. Bleeding may happen if small blood vessels near a pouch rupture, sometimes leading to noticeable blood in stools.
In rare cases, a pouch might rupture, spilling intestinal contents into the abdominal cavity and causing a serious infection called peritonitis. Repeated infections can lead to scar tissue that narrows the colon or creates abnormal connections between organs called fistulas. These complications require prompt medical treatment.
Dietary Management Approaches
Fiber forms the cornerstone of managing diverticulosis. Gradually increasing fiber intake to 25-35 grams daily helps soften stool and reduce pressure in the colon. Good sources include whole grains, fruits, vegetables, and legumes. Adding fiber slowly prevents gas and bloating while your system adjusts.
Staying well-hydrated makes fiber more effective. Water helps fiber form soft, bulky stools that pass easily. Some people benefit from probiotics found in yogurt and fermented foods, though research on their specific benefit for diverticulosis remains ongoing.
When Treatment Becomes Necessary
Uncomplicated diverticulosis requires no specific treatment beyond dietary adjustments. Doctors may recommend fiber supplements if dietary changes prove insufficient. For those with occasional mild symptoms, over-the-counter pain relievers like acetaminophen may help, though avoiding regular NSAID use is wise as these medications may increase bleeding risk.
Antispasmodic medications can ease cramping for some patients. Unlike diverticulitis which may require antibiotics or surgery, diverticulosis management focuses primarily on prevention of complications through lifestyle measures.
The Role of Exercise in Prevention
Regular physical activity appears protective against diverticular complications. Exercise stimulates normal bowel function and reduces pressure in the colon. Aim for at least 30 minutes most days – even walking counts. Activity also helps maintain healthy weight, another factor in diverticular health.
Yoga and other exercises that gently massage the abdomen may be particularly helpful. The key is consistency rather than intensity – making movement a regular habit supports overall colon health.
Monitoring and Follow-Up Care
For those diagnosed with diverticulosis, routine follow-up typically involves monitoring for any new symptoms rather than frequent testing. Report any persistent abdominal pain, major changes in bowel habits, or rectal bleeding to your doctor promptly.
People with a history of diverticular bleeding may need periodic blood tests to check for anemia. Those who’ve had previous diverticulitis episodes require closer monitoring for recurrence. Otherwise, diverticulosis alone rarely needs extensive medical follow-up.
Surgical Considerations
Surgery isn’t indicated for uncomplicated diverticulosis. Even multiple diverticula don’t warrant removal unless severe complications develop. For recurrent diverticulitis or serious cases involving abscesses or perforations, surgeons may remove the affected colon section.
These decisions are highly individual, weighing factors like attack frequency, severity, and overall health. Most people with diverticulosis will never need surgery related to their condition.
The Emotional Aspect of Diagnosis
Learning you have diverticulosis can cause unnecessary worry if not properly understood. Many patients fear imminent complications or drastic lifestyle changes upon diagnosis. In reality, most continue life normally with simple dietary adjustments.
Focusing on controllable factors like diet and exercise provides empowerment. Support groups can help those struggling with anxiety about their condition, though many find reassurance simply in understanding how common and typically benign diverticulosis truly is.
Future Research Directions
Scientists continue studying why some people develop complications while most don’t. Investigations into gut bacteria’s role may explain why certain individuals progress to diverticulitis. New research explores whether anti-inflammatory diets could prevent flare-ups in susceptible people.
Some studies examine potential medications to strengthen colon walls or modify gut flora. As understanding grows, more targeted prevention strategies may emerge, but currently, fiber remains the best evidence-based approach.
Conclusion
The key message about diverticulosis is that it’s generally a harmless structural change rather than a disease. Most people live full lives without ever experiencing problems from their diverticula. Simple preventive measures can significantly reduce already low risks of complications.
Rather than fearing diverticulosis, view it as motivation to adopt healthier habits that benefit your entire body. Eating more fiber, staying active, and maintaining good hydration support not just colon health but overall wellbeing. With this perspective, diverticulosis becomes just one of many normal changes that come with aging, not a reason for concern.
Related topics:
What Is Systolic Hypertension?
How Is Foot-And-Mouth Disease Transmitted?