Bipolar disorder is a complex mental health condition characterized by extreme shifts in mood, energy, and behavior. Traditionally, it has been classified into distinct types, such as Bipolar I and Bipolar II. However, growing research suggests that bipolar disorder may not fit neatly into these categories. Instead, it may exist on a spectrum, with symptoms varying widely in intensity and presentation.
This article explores the concept of bipolar disorder as a spectrum disorder. We will examine the evidence supporting this idea, the different manifestations of bipolar symptoms, diagnostic challenges, and treatment approaches. By the end, you will have a clearer understanding of why many experts now view bipolar disorder as a continuum rather than a set of rigid diagnoses.
Understanding Bipolar Disorder
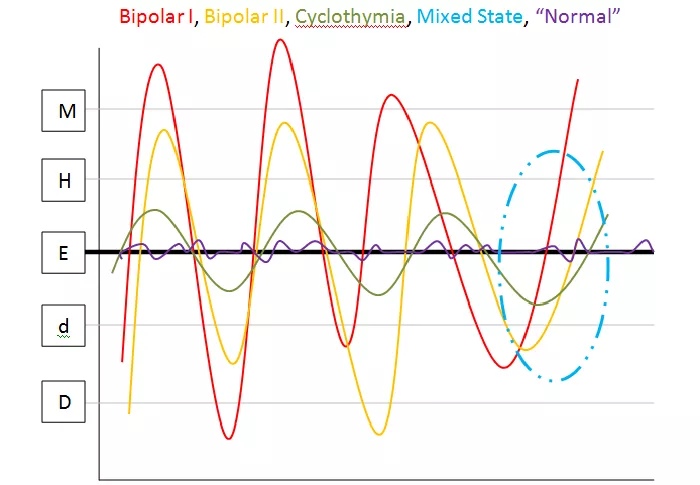
Bipolar disorder is marked by episodes of mania (or hypomania) and depression. These episodes can significantly impact a person’s daily life, relationships, and overall functioning. The primary types of bipolar disorder include:
Bipolar I Disorder: Defined by at least one full manic episode, often accompanied by severe depression.
Bipolar II Disorder: Characterized by hypomania (a milder form of mania) and major depressive episodes.
Cyclothymic Disorder: A chronic but less severe form, with frequent mood fluctuations that do not meet the full criteria for mania or major depression.
Other Specified and Unspecified Bipolar Disorders: Cases where symptoms do not fit the classic definitions but still cause significant distress.
The variability in symptom severity and presentation has led researchers to question whether bipolar disorder is better understood as a spectrum.
The Spectrum Model of Bipolar Disorder
The spectrum model proposes that bipolar disorder is not a single, uniform condition but rather a range of related disorders with overlapping symptoms. This perspective acknowledges that mood disorders exist on a continuum, with some individuals experiencing mild symptoms and others facing severe, disabling episodes.
Evidence Supporting the Spectrum Theory
Symptom Variability
Some people experience extreme mania with psychosis, while others have only mild hypomania. Similarly, depressive episodes can range from moderate to life-threatening. This wide variation suggests a spectrum rather than fixed categories.
Overlap With Other Mental Health Conditions
Bipolar disorder shares symptoms with conditions like major depressive disorder, ADHD, and borderline personality disorder. Many patients are initially misdiagnosed because their symptoms do not align perfectly with traditional bipolar classifications.
Genetic and Neurobiological Factors
Studies show that bipolar disorder has a strong genetic component, but not everyone with a family history develops the same symptoms. Brain imaging studies also reveal differences in individuals with bipolar disorder, but these differences are not consistent across all cases.
Treatment Response Variability
Some individuals respond well to mood stabilizers like lithium, while others require a combination of medications and therapy. This variability suggests that different biological mechanisms may be at play across the spectrum.
Challenges to the Spectrum Model
Despite the growing acceptance of the spectrum model, some experts remain cautious. Key concerns include:
Diagnostic Clarity: Clear criteria for bipolar I and II help guide treatment. A spectrum approach might blur these lines, leading to confusion in diagnosis.
Risk of Overdiagnosis: Labeling normal mood swings as part of a bipolar spectrum could lead to unnecessary medicalization.
Treatment Implications: Without clear categories, developing standardized treatment guidelines becomes more challenging.
However, many clinicians find the spectrum model useful for identifying and treating patients who do not fit traditional diagnostic boxes.
Symptoms Across the Bipolar Spectrum
Bipolar symptoms can manifest in diverse ways, depending on where a person falls on the spectrum.
Manic and Hypomanic Symptoms
- Elevated or irritable mood
- Increased energy and decreased need for sleep
- Racing thoughts and rapid speech
- Impulsive or risky behaviors (e.g., excessive spending, reckless driving)
- Grandiose beliefs or inflated self-esteem
Depressive Symptoms
- Persistent sadness or hopelessness
- Loss of interest in activities once enjoyed
- Fatigue and low energy
- Difficulty concentrating or making decisions
- Thoughts of death or suicide
Mixed Episodes
Some individuals experience symptoms of mania and depression simultaneously, leading to agitation, irritability, and emotional turmoil.
Diagnosing Bipolar Disorder: Challenges and Considerations
Accurate diagnosis can be difficult due to the overlapping symptoms with other disorders. Mental health professionals use several methods to assess bipolar disorder:
Clinical Interviews: A thorough discussion of mood history, family background, and behavioral patterns.
Mood Tracking: Patients may keep a daily mood journal to identify patterns over time.
Rule-Out Procedures: Medical tests to exclude conditions like thyroid disorders or substance abuse that can mimic bipolar symptoms.
The spectrum model helps clinicians recognize subtler forms of bipolar disorder that might otherwise be missed.
Treatment Approaches for Bipolar Spectrum Disorders
Treatment must be tailored to the individual’s specific symptoms and needs.
Common strategies include:
Medication Management
Mood Stabilizers: Lithium, valproate, and lamotrigine help regulate mood swings.
Antipsychotics: Aripiprazole, quetiapine, and olanzapine can manage manic or mixed episodes.
Antidepressants: Used cautiously, as they may trigger manic episodes in some individuals.
Psychotherapy
Cognitive Behavioral Therapy (CBT): Helps patients identify and change negative thought patterns.
Family-Focused Therapy: Educates family members on supporting their loved one.
Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines to prevent mood episodes.
Lifestyle Modifications
- Maintaining a regular sleep schedule
- Engaging in regular physical activity
- Avoiding alcohol and recreational drugs
- Practicing stress-reduction techniques like mindfulness or yoga
Hospitalization in Severe Cases
Necessary for individuals experiencing psychosis, severe mania, or suicidal thoughts.
Living With Bipolar Disorder: Strategies for Stability
Managing bipolar disorder requires ongoing effort, but stability is achievable with the right approach. Key strategies include:
Adhering to Treatment: Skipping medications or therapy can trigger relapses.
Monitoring Mood Changes: Early recognition of symptoms can prevent full-blown episodes.
Building a Support System: Friends, family, and support groups provide crucial encouragement.
Reducing Stress: High stress can worsen symptoms, so relaxation techniques are essential.
Conclusion
The idea of bipolar disorder as a spectrum offers a more nuanced understanding of this condition. Rather than forcing patients into rigid categories, the spectrum model acknowledges the diversity of experiences and allows for more personalized treatment.
While debates continue, the spectrum approach has already improved diagnosis and care for many individuals. If you or someone you know struggles with mood instability, seeking professional evaluation is the first step toward effective management.
Related topics:
- What Is Bipolar Disorder With Psychotic Features?
- Wondering If You Have Bipolar Disorder? Here’s How To Test
- Why ADHD Is Not Considered To Be On The Spectrum?