Hormone replacement therapy (HRT) has been a cornerstone in the management of various hormonal imbalances and menopausal symptoms for decades. With the aging population and increasing awareness about hormonal health, the demand for HRT has soared. Among the plethora of HRT options available, one particular regimen stands out as the most commonly prescribed. In this article, we delve into the intricacies of this widely used HRT, exploring its mechanisms, indications, benefits, and potential risks.
Understanding HRT
HRT, also known as menopausal hormone therapy (MHT) or postmenopausal hormone therapy (PHT), involves the administration of hormones to supplement or replace those that the body no longer produces in adequate amounts. The primary hormones addressed in HRT are estrogen and progesterone, although testosterone and thyroid hormones may also be included in certain formulations.
The Rise of Estrogen-Progestin Therapy
Estrogen-progestin therapy, commonly referred to as combination HRT, has emerged as the most frequently prescribed form of hormone replacement. This regimen typically includes a combination of estrogen and progestin, a synthetic form of progesterone. Estrogen-progestin therapy is predominantly used in postmenopausal women, especially those who have not undergone hysterectomy.
Indications for Estrogen-Progestin Therapy
The indications for estrogen-progestin therapy are manifold, encompassing both symptomatic relief and disease prevention.
Menopausal Symptom Management: Estrogen-progestin therapy effectively alleviates menopausal symptoms such as hot flashes, night sweats, vaginal dryness, and mood swings, significantly enhancing the quality of life for many women transitioning through menopause.
Prevention of Osteoporosis: Estrogen plays a crucial role in maintaining bone density. Estrogen-progestin therapy helps prevent osteoporosis and reduce the risk of fractures in postmenopausal women, particularly those with a high risk of bone loss.
Cardiovascular Protection: There is evidence to suggest that estrogen-progestin therapy may confer cardiovascular benefits, including a reduced risk of coronary artery disease and stroke, particularly when initiated early in menopause.
Urogenital Health: Estrogen-progestin therapy improves urogenital health by restoring vaginal lubrication, elasticity, and pH balance, thereby alleviating symptoms of vaginal atrophy and reducing the risk of urinary tract infections.
Management of Vasomotor Symptoms: The vasomotor symptoms associated with menopause, such as hot flashes and night sweats, are effectively managed with estrogen-progestin therapy, enhancing overall comfort and well-being.
Formulations of Estrogen-Progestin Therapy
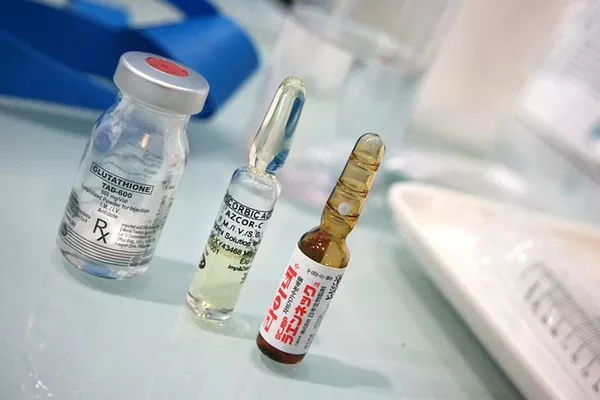
Estrogen-progestin therapy is available in various formulations, including oral tablets, transdermal patches, gels, and vaginal creams. Each formulation offers distinct advantages in terms of convenience, efficacy, and side effect profile.
Oral Tablets: Oral estrogen-progestin tablets are the most commonly prescribed formulation due to their convenience and ease of administration. They are available in different estrogen-progestin combinations and dosage strengths to cater to individual patient needs.
Transdermal Patches: Transdermal estrogen-progestin patches provide a steady release of hormones through the skin, bypassing the gastrointestinal tract and liver metabolism. This route of administration may be preferred for women who experience gastrointestinal intolerance or prefer to avoid oral medications.
Topical Gels: Estrogen-progestin gels offer a non-oral alternative for hormone delivery, allowing for precise dosing and absorption through the skin. These gels are typically applied to the arms, abdomen, or thighs and offer the flexibility of adjusting the dosage as needed.
Vaginal Creams: Vaginal estrogen-progestin creams are primarily used to address urogenital symptoms such as vaginal dryness, itching, and dyspareunia. They are applied directly to the vaginal mucosa and are effective in restoring vaginal health and comfort.
Benefits of Estrogen-Progestin Therapy
Estrogen-progestin therapy offers a multitude of benefits, making it a preferred choice for many women undergoing menopause or experiencing hormonal imbalances. Some of the key benefits include:
Effective Symptom Relief: Estrogen-progestin therapy provides rapid and significant relief from menopausal symptoms, allowing women to regain control over their lives and daily activities.
Bone Health: By preventing bone loss and reducing the risk of fractures, estrogen-progestin therapy helps maintain skeletal integrity and mobility in postmenopausal women, promoting long-term bone health.
Cardiovascular Protection: Despite some controversies surrounding the cardiovascular risks associated with HRT, estrogen-progestin therapy has been shown to have favorable effects on lipid profiles, endothelial function, and arterial stiffness, potentially reducing the risk of cardiovascular events.
Improved Quality of Life: Relief from bothersome menopausal symptoms, enhanced urogenital health, and improved bone density contribute to an overall improvement in quality of life for women receiving estrogen-progestin therapy.
Risks and Considerations
While estrogen-progestin therapy offers significant benefits, it is not without risks. It is essential for healthcare providers and patients to weigh the potential risks against the benefits and individualize treatment decisions based on each woman’s medical history, risk factors, and preferences.
Breast Cancer Risk: Long-term use of estrogen-progestin therapy has been associated with a slight increase in the risk of breast cancer. Women considering HRT should undergo thorough risk assessment and regular breast cancer screening.
Venous Thromboembolism: Estrogen-progestin therapy may increase the risk of venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), particularly in women with preexisting risk factors such as obesity, smoking, or a personal or family history of VTE.
Cardiovascular Risks: Although estrogen-progestin therapy has been linked to cardiovascular benefits, there is conflicting evidence regarding its long-term effects on cardiovascular health. Women with a history of cardiovascular disease or risk factors such as hypertension, diabetes, or hyperlipidemia should discuss the potential risks and benefits of HRT with their healthcare providers.
Endometrial Hyperplasia and Cancer: Unopposed estrogen therapy (without progestin) increases the risk of endometrial hyperplasia and endometrial cancer. Adding progestin to estrogen therapy mitigates this risk by inducing regular menstrual bleeding and shedding the endometrial lining.
Conclusion
Estrogen-progestin therapy remains the most commonly prescribed form of hormone replacement therapy for menopausal symptom management and disease prevention. Despite the controversies surrounding its risks and benefits, estrogen-progestin therapy continues to play a crucial role in improving the quality of life and overall health outcomes for countless women worldwide. By understanding the indications, formulations, benefits, and potential risks associated with estrogen-progestin therapy, healthcare providers can empower women to make informed decisions about their hormonal health and well-being.
FAQs
Q1: What are the names of HRT medications?
Common hormone replacement therapy (HRT) medications include estradiol, conjugated equine estrogen (CEE), progesterone, medroxyprogesterone acetate (MPA), micronized progesterone, and testosterone. These medications come in various forms such as pills, patches, gels, creams, and injections.
Q2: What is the best lowest risk HRT?
There isn’t a universally agreed-upon “best” HRT with the lowest risk for everyone, as it depends on individual health factors and preferences. Generally, transdermal estrogen (via patches or gels) is considered to have lower risks of blood clots and stroke compared to oral estrogen, especially in older women or those with certain health conditions. Bioidentical hormones are often preferred by some individuals, as they are chemically identical to hormones produced by the body.
Q3: What do doctors prescribe for HRT?
Doctors commonly prescribe hormone replacement therapy (HRT) based on individual patient needs and health considerations. This may include estrogen (such as estradiol or conjugated equine estrogen), progesterone (such as micronized progesterone or medroxyprogesterone acetate), or testosterone. The specific medication and dosage depend on factors like menopausal status, symptoms, medical history, and personal preferences.
Related topics:
- Natural Remedies for Hot Flashes: Managing Menopausal Symptoms
- HRT: Identifying the Safest Progesterone Options
- Navigating Perimenopause: How Vitamins Can Provide Relief