A recent study has uncovered significant disparities in dementia diagnosis and treatment across different regions of the United States. The findings highlight not only geographic inequities but also reveal that certain populations, particularly Black and Hispanic individuals, as well as those aged 66-74, are more likely to be underdiagnosed.
The variations in diagnosis rates are likely due to a complex web of factors that overlap in various ways. The study suggests that individuals in certain areas of the U.S. are significantly less likely to receive a timely diagnosis and appropriate treatment for dementia compared to others. These discrepancies are particularly pronounced among historically marginalized groups, according to the study published in Alzheimer’s & Dementia.
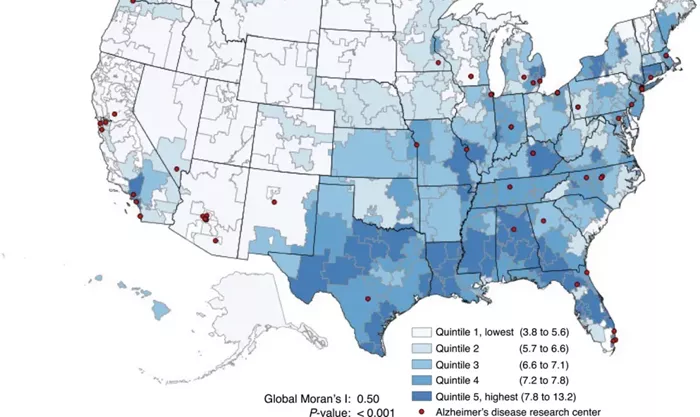
The researchers analyzed Medicare Fee-for-Service records for 4,842,034 older beneficiaries from 2018 to 2019 to assess the diagnosis rates of Alzheimer’s disease and related dementias (ADRD). The study found that the likelihood of receiving a dementia diagnosis varied greatly depending on the region, irrespective of common population risk factors such as education level, obesity, smoking habits, and diabetes.
The intensity of dementia diagnosis in different hospital referral regions ranged widely, from 0.69 to 1.47, demonstrating a stark contrast in how dementia is recognized and treated across the country. The disparities were most evident among Black and Hispanic populations and those in the 66-74 age group, who were the youngest likely to be affected by dementia.
Exploring the Causes Behind Diagnostic Discrepancies
Lycia Neumann, Ph.D., senior director of Health Services Research at the Alzheimer’s Association of America, who was not involved in the study, emphasized that Alzheimer’s and other dementias are frequently underdiagnosed. She pointed out that the 2024 Alzheimer’s Disease Facts and Figures report aligns with the new study’s findings, showing significant geographical differences in dementia diagnosis rates exacerbated by age and racial/ethnic disparities.
The study’s lead author, Dr. Julie P. W. Bynum, a professor of geriatric and palliative medicine at Johns Hopkins School of Medicine, acknowledged that the data alone could not definitively identify the root causes of these differences. However, she suggested that variations in healthcare systems serving different communities are likely contributors. These include factors such as the confidence and comfort level of primary care providers in making dementia diagnoses and the availability of dementia specialists to manage more complex cases.
Dr. Bynum also speculated that patient and family attitudes might influence these discrepancies. She noted that beliefs about dementia, such as seeing it as a normal part of aging, concerns about stigma, or the perception that little can be done to help, could deter people from seeking a diagnosis.
Neumann added that other complicating factors, such as limited healthcare access due to inadequate insurance coverage, distance from clinical facilities, and lack of transportation and companionship, further exacerbate the issue.
Populations Most at Risk of Underdiagnosis
For Black and Hispanic individuals, Dr. Bynum explained, there are numerous studies across various diseases showing lower access to healthcare, lower levels of care-seeking, and underdiagnosis—all of which also apply to dementia. She also noted that stigma related to a dementia diagnosis is often more pronounced in these communities, which can prevent individuals from pursuing a diagnosis.
Older individuals in the 66-74 age group face additional challenges. Dr. Bynum pointed out that clinicians may be less likely to suspect dementia in this younger cohort since it is less common. Furthermore, early-stage dementia can be difficult to diagnose as symptoms may be subtle and easily mistaken for other conditions, such as depression. Additionally, individuals who are still working may avoid seeking a diagnosis due to concerns about its impact on their careers.
Implications and Potential Solutions
Neumann praised the study for providing valuable data that could inform efforts to address these disparities. By integrating claims data with spatial analysis, the study offers a clearer understanding of the inequities in access to dementia care, beginning with diagnosis. This objective data is crucial for developing educational programs and systemic changes that can improve diagnosis rates equitably.
However, Neumann cautioned that the study is based on data from 2018-2019. She expressed hope that advancements in diagnostic tools, such as less invasive and more affordable blood tests, could enhance access to diagnosis in the future. She highlighted the Alzheimer’s Association’s role in funding research that has led to significant progress in diagnosis through advanced imaging and fluid biomarkers.
The Alzheimer’s Association is also actively working to increase awareness of dementia’s signs and symptoms and to improve access to and the quality of diagnosis, treatment, and care. Neumann is one of the chairs of a multidisciplinary scientific committee that will convene in November 2024 for a conference on “Exploring Equity in Diagnosis.” This event aims to bring together experts to advance research and collaboration on addressing disparities in dementia diagnosis.
Steps to Take in Underserved Areas
For individuals living in areas where dementia concerns are not being adequately addressed, there are proactive steps that can be taken. Educating oneself about the signs of dementia is a critical first step. Additionally, seeking out specialized medical experts, even beyond one’s usual healthcare providers, may be necessary. Community organizations, senior centers, or nearby Alzheimer’s Association chapters can also provide valuable guidance and resources for those navigating the challenges of a dementia diagnosis.
Related Articles:
Is Dementia a Psychological Condition?
A Comprehensive Guide to Dementia-Related Psychosis
Social Disparity: Survey Reveals Adults Without Degrees Often Friendless